![]() I’ve stated before that I am firmly in the cognitive-behavioral therapy (CBT) camp. I read in a paper assigned for my last class that people do not choose theoretical orientation die to efficacy. I disagree. I initially started reading books by Aaron Beck and Albert Ellis because CBT has a wealth of research behind it, and I found that it just seemed to make logical sense.
I’ve stated before that I am firmly in the cognitive-behavioral therapy (CBT) camp. I read in a paper assigned for my last class that people do not choose theoretical orientation die to efficacy. I disagree. I initially started reading books by Aaron Beck and Albert Ellis because CBT has a wealth of research behind it, and I found that it just seemed to make logical sense.
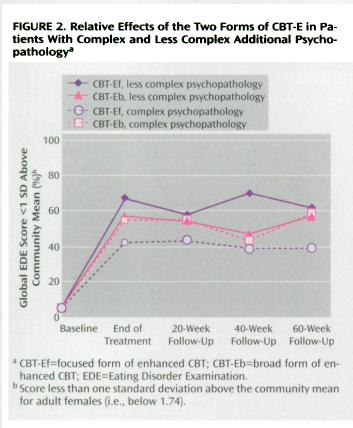
In a randomized controlled study by Fairburn et al. published in the American Journal of Psychiatry, researchers studied the use of a specific form of CBT designed to treat eating disorders. There are two forms of the therapy, CBT-Ef, which is a focused form that highlights issues directly related to eating disorders such as body image, extreme dieting, binging, and purging, and CBT-Eb, a broad form which also touches on other psychopathology, such as depression, low self-esteem, mood intolerance, and interpersonal difficulties.
When the results were tallied, researchers looked at complex psychopathology and simple psychopathology. Subjects in the complex psychopathology group tended to be assessed as having more mood intolerance, interpersonal difficulties, and self-esteem issues. The results are kind of interesting:
As you can see from the graph, CBT-Ef works best with simple psychopathology, but does not work nearly as well with complex psychopathology. The CBT-Eb group shows similar results with both simple and complex psychopathology.
It looks like the focused approach is not really necessary, but can give better results when used with clients with less complex psychopathology. The broad approach seems to be preferable, but less effective.
This study shows us the importance of clinical judgment. Clinicians need to be able to assess the complexity of their clients’ psychopathology in order to find the right emphasis for therapy. In these two therapies, the first four weeks are the same regardless of whether a clinician is using the focused or broad approach, giving clinicians plenty of time to assess their clients’ needs.
Fairburn, C., Cooper, Z., Doll, H., O’Connor, M., Bohn, K., Hawker, D., Wales, J., & Palmer, R. (2009). Transdiagnostic Cognitive-Behavioral Therapy for Patients With Eating Disorders: A Two-Site Trial With 60-Week Follow-Up American Journal of Psychiatry, 166 (3), 311-319 DOI: 10.1176/appi.ajp.2008.08040608



 Posted by Danny McCaslin
Posted by Danny McCaslin